The 5-Pill Tipping Point: Uncovering the Hidden Medication Risks Endangering Your Parents
The biggest fall risk for your parents could be hiding in plain sight, right in their medicine cabinet. We often attribute unsteadiness, dizziness, or confusion to the normal process of "just getting older." However, these can be red flags for a serious, yet often overlooked, condition: polypharmacy.
Polypharmacy is the concurrent use of five or more medications, and it represents a critical tipping point where the risk of adverse medical events, especially falls, doesn't just increase—it accelerates.
The 5-Pill Tipping Point: When More is Not Merrier
Clinical data reveals a stark reality about medication management in older adults. While each prescription is given with good intention, the cumulative load on the body’s systems can create a cascade of unintended consequences. This isn’t about a single "bad" drug; it's about the sheer volume. Once a person crosses the threshold of five regular medications, their risk of falls, frailty, and other adverse outcomes grows disproportionately.
This is the "5-Pill Tipping Point." It’s a crucial metric that shifts the focus from individual prescriptions to the systemic risk of the entire regimen. Recognizing this number is the first step for any caregiver to begin managing that risk proactively.

The "1+1=3" Effect: Unmasking Hidden Drug Interactions
How can medications that are safe on their own become dangerous when combined? The answer lies in how our bodies process them, which can be explained with a simple analogy: The "Traffic Jam" in your liver.
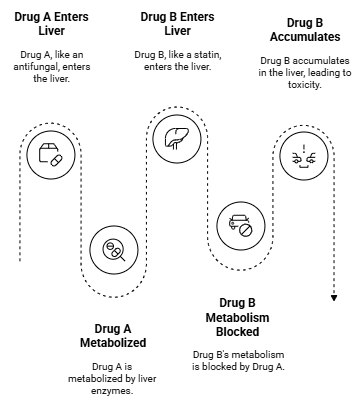
Think of your liver's enzymes as toll booths on a highway, breaking down drugs so they can exit your body. Now, imagine you take "Drug A," and it unexpectedly closes down a specific toll booth. If "Drug B" needs that exact same toll booth to be processed, it gets stuck. As you continue taking your daily dose, Drug B creates a massive traffic jam, building up to potentially toxic levels.
This is a real biological process called metabolic inhibition. The effect isn't just additive; it's synergistic. This "1+1=3" effect is why two seemingly safe medications can create an unpredictable and dangerous combination, leading to side effects like dizziness, confusion, or instability—major drivers of falls. Understanding this mechanism is key to becoming a better advocate.
From Passive Patient to Proactive Advocate: The 3-Step Medication Audit
The goal is not to self-diagnose or play pharmacist. It is to shift from a passive observer to a proactive "project manager" of your parent's health. By conducting a thorough medication audit before a doctor's visit, you can provide the medical team with crucial on-the-ground data they may not possess. This approach empowers you to ask better questions and ensure a safer therapeutic environment.
Framing this process as preparation for a doctor's visit is essential. Any potential changes to a medication routine must be discussed with and directed by a physician.
Here is a 3-step strategy to prepare for that critical conversation:
- INVENTORY: Gather every single prescription medication, over-the-counter (OTC) drug, and supplement your parent takes. Create a comprehensive list, including dosages and frequency.
- FLAG: Identify potential risks. While you are not expected to be an expert, you can note medications known to cause dizziness or drowsiness. Discussing the reduction of high-risk drug classes, such as those on the AGS Beers Criteria®, with your parent's physician can be a key step in improving balance and safety.
- REVIEW: Prepare a concise list of questions and concerns. Focus on the "why"—why is each medication prescribed, are there non-pharmacological alternatives, and could any symptoms be related to drug interactions?
By building this dossier, you provide the doctor with the intelligence needed to make the best possible decisions. You're not making the medical calls; you are ensuring the architect has the complete blueprint.